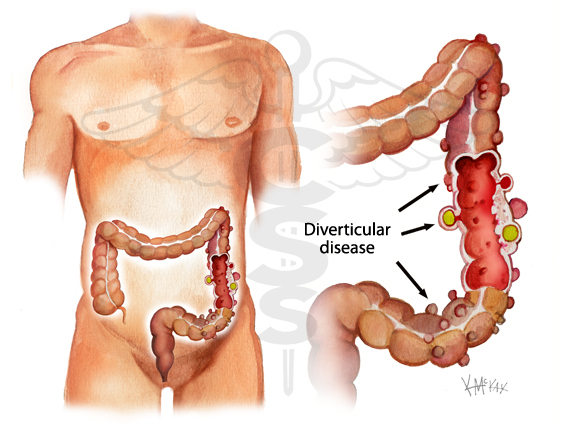
It's not known exactly why some people get diverticular disease, but it seems to be linked to age, diet and lifestyle, and genetics.
Age
As you get older, the walls of your large intestine become weaker and the pressure of hard stools passing through your intestines can cause diverticula to form.
The majority of people will have some diverticula by the time they are 80 years old.
Diet and lifestyle
Not eating enough fibre is thought to be linked to developing diverticular disease and diverticulitis.
Fibre helps to make your stools softer and larger, so they put less pressure on the walls of your intestines.
Some other things that seem to increase your risk include:
smoking
being overweight or obese
having a history of constipation
long-term regular use of painkillers such as ibuprofen or aspirin



 Contact Us
Contact Us




 Hospitals
Hospitals
 Doctors
Doctors
 Diagnostic
Diagnostic
 Pharmacy
Pharmacy
 Health Tips
Health Tips
 Blog
Blog























Comments